Time in range is the percentage of time your blood sugar level is within a ‘target’ range. The target range is decided with your healthcare team and this range will vary from person to person.
For many people the target range is 3.9mmol/l to 10mmol/l. Time in range is not a replacement for HbA1c, which is another way to measure blood sugar levels.
The benefits of being within an ‘ideal’ or ‘target’ range over time means your diabetes management will improve, and you will be less likely to develop diabetes complications from high blood sugar levels.
Time in range v HbA1c
The most common way to measure ‘safe’ ranges in blood sugar levels is your HbA1c blood test, which measures your average blood sugar levels for the last 2-3 months.
Although HbA1c doesn’t give you an understanding of what your blood sugar levels are at all times, it’s an effective way of measuring your risk of getting diabetes complications from high blood sugar levels.
Using time in range together with HbA1c can be an effective way for your healthcare team to review your diabetes care to help you reduce your risk of long-term health problems.
What is my recommended time in range?
Time in range targets will be different for everyone. Most diabetes experts say that a target range of 3.9-10 mmol/L is recommended for people with diabetes, with the aim of being in this target range for at least 70% of the day.
However, considerations such as diabetes type, age, pregnancy and other health conditions will need to be considered by your diabetes team.
You should talk to your diabetes team about what the best time in range target is for you.
Diabetes technology and time in range
Diabetes technology, such as insulin pumps, continuous glucose monitors (CGM) and closed loop systems can be used to increase your time in range.
Using a CGM either in combination with an insulin pump or with multiple daily injections enables people with diabetes to monitor their time in range.
If you use a hybrid closed loop system, you might find it’s improved your time in range because the amount of insulin given is calculated more precisely and given more often. This can help keep your blood sugar levels stable and increase the amount of time in range.
Time in range and CGM
If you use a CGM, which provides information on your glucose levels 24 hours a day, you can find out what your time in range is every day.
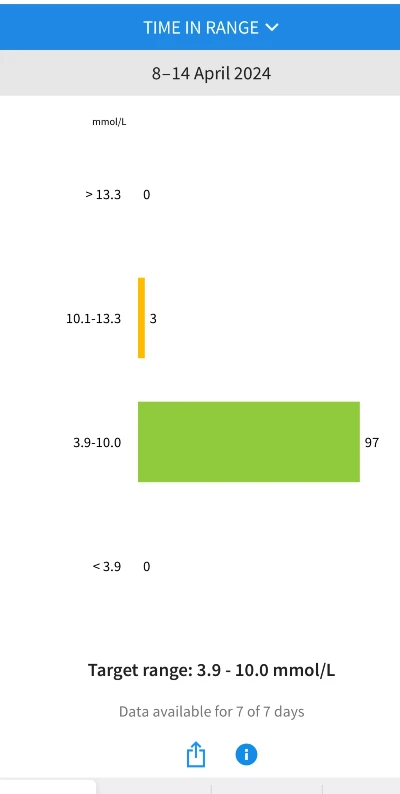
Time in range is usually displayed as a bar graph which you can view on the app that you use with your CGM sensor on your mobile phone. This data can also be shared with your healthcare team.
If you use a reader with your CGM you’ll be able to view this information on the reader.
These bar graphs show the percentage of time when your sugar levels were:
- low – time below range (TBR)
- in range – time in range (TIR)
- high – time above range (TAR).
This data can also help you and your health care team to spot patterns and trends, and the effects of food, physical activity, and the timing of insulin injections on your sugar levels.
This information can help you and your healthcare team make decisions about things that might need to be changed to increase your time in range.
The data might also help you to spot hypos overnight that haven’t woken you up. These hypos overnight can then push your blood sugar levels up during the day. So if you notice this is a regular pattern, it may help to talk to your diabetes team about potentially reducing your overnight insulin.
How to increase your time in range
Generally, if your time in range is high, your HbA1c is more likely to be in the target range, too.
There are a few ways you can increase your time in range. Below are a few examples, but it’s best to speak to your diabetes team to work out an individualised plan.
You could also ask your healthcare team to refer you to a diabetes education course to learn more about insulin doses and time in range.
Reducing hypoglycaemia
Reducing the amount of time your blood sugar levels are low, also called hypoglycaemia or hypos, is an important part of diabetes management.
Reducing the amount of time you’re below range can help to increase your time in range.
The data you get from a CGM can tell you how often or how long you’ve had hypos for. You might also be able to work out why your sugar levels dropped and identify patterns. You can review this data with your diabetes team who can advise you on any treatment changes you might need to make.
As CGMs can show you whether your sugar levels are going up or down, this can help you prevent hypoglycaemia. For example, you could eat some fast-acting carbohydrate. Read more about treating low blood sugar.
You can also set alarms on your CGM to alert you when your blood sugar levels are going low or high.
Exercise
Being physically active is important for everyone living with diabetes.
Exercise can help insulin work better in your body – either the insulin you take or the insulin your body makes. This can help keep your blood sugar levels within target and improve your time in range.
You don’t need to join a gym to be physically active – even walking on the spot at home can make a difference. What’s important is you’re getting your body moving.
Eating well
There’s no specific diabetes diet, but eating a healthy, balanced diet can help with blood sugar level management and improve your time in range.
Eating well can also improve how you feel and how much energy you have.
It’s important to know the impact each of the main food groups can have on your blood sugar levels and overall health.
For example, all carbs you eat and drink are broken down into glucose so it’s important to know which foods contain carbohydrates. The type, and amount you consume, can make a difference to your blood sugar levels and diabetes management.
Stress management
We all feel stressed from time-to-time, whether that’s over something short-term, like preparing for a job interview, or more constant worries, like about money or a relationship.
Stress can affect your blood sugar levels, but there are things you can do to cope to help prevent it from impacting your overall time in range, and your emotional health.
When you’re stressed, your body releases hormones like cortisol and adrenaline. These prepare you for a ‘fight or flight response’. But they can also make it harder for the insulin in your body to work properly. This can lead to your blood sugar levels rising and your time in range decreasing.
